Diabetes Care:新型“明星药”达格列净能有效预防并治疗糖尿病肾脏疾病
2021-08-28 MedSci原创 MedSci原创
蛋白尿经常是糖尿病肾病的一个组成部分。
蛋白尿经常是糖尿病肾病的一个组成部分。在观察性研究和临床试验中,无论是否患有糖尿病,蛋白尿的存在都与不良肾脏和心血管(CV)结果的风险增加有关,而蛋白尿的减少则与不良肾脏和CV结果的发生率降低有关。为此,美国糖尿病协会的《糖尿病医疗护理标准》建议作为2型糖尿病患者实验室筛查的一部分,每年检测尿蛋白排泄量。
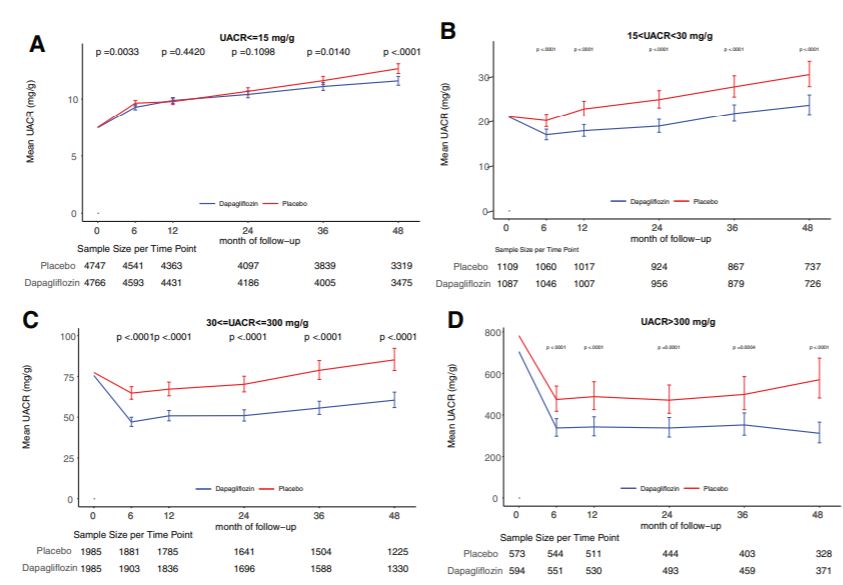
钠-葡萄糖共转运体2抑制剂(SGLT2i)可降低2型糖尿病患者的不良肾脏结果的风险,包括减少估计肾小球滤过率(eGFR)的恶化和进展到终末期肾脏疾病(ESKD)。这已被证明是CV结果试验(CVOTs)的重要研究结果,并被确认为蛋白尿慢性肾脏病(CKD)患者的主要结果。
达格列净对心血管事件的影响试验(DECLARE-TIMI 58)是一项针对17160名2型糖尿病患者和动脉粥样硬化性心血管疾病(ASCVD)(59.4%)或已确定的ASCVD(eASCVD)(40.6%)的CVOT,证明其CV死亡和心衰住院这两个主要疗效结果中的一个显著减少17%。
近期,来自以色列哈达萨医疗中心内分泌和代谢部的专家公布了达格列净对心血管事件的影响(DECLARE-TIMI 58)心血管结果试验中蛋白尿的变化,该试验包括心肾风险较低的人群。结果发表在《糖尿病护理》Diabetes Care杂志上。
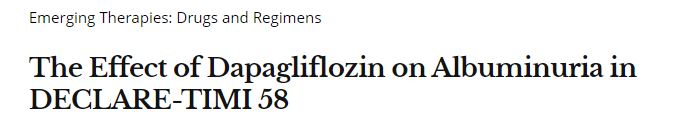
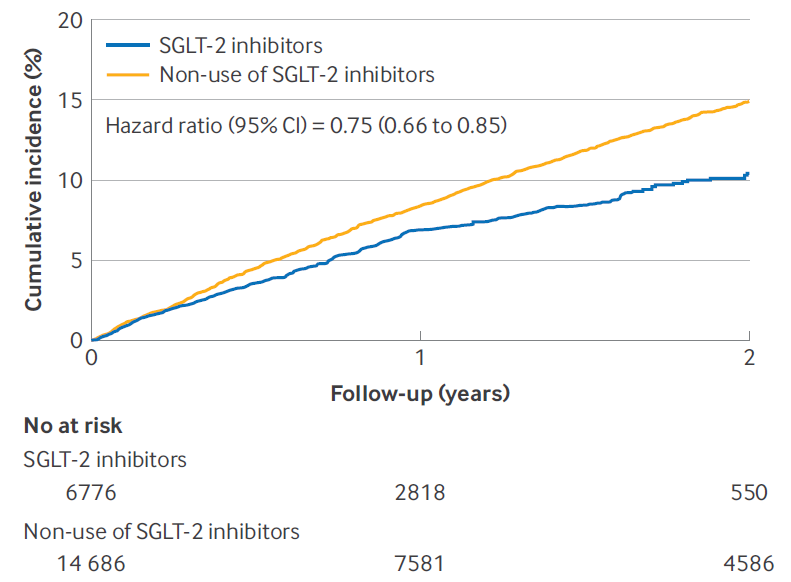
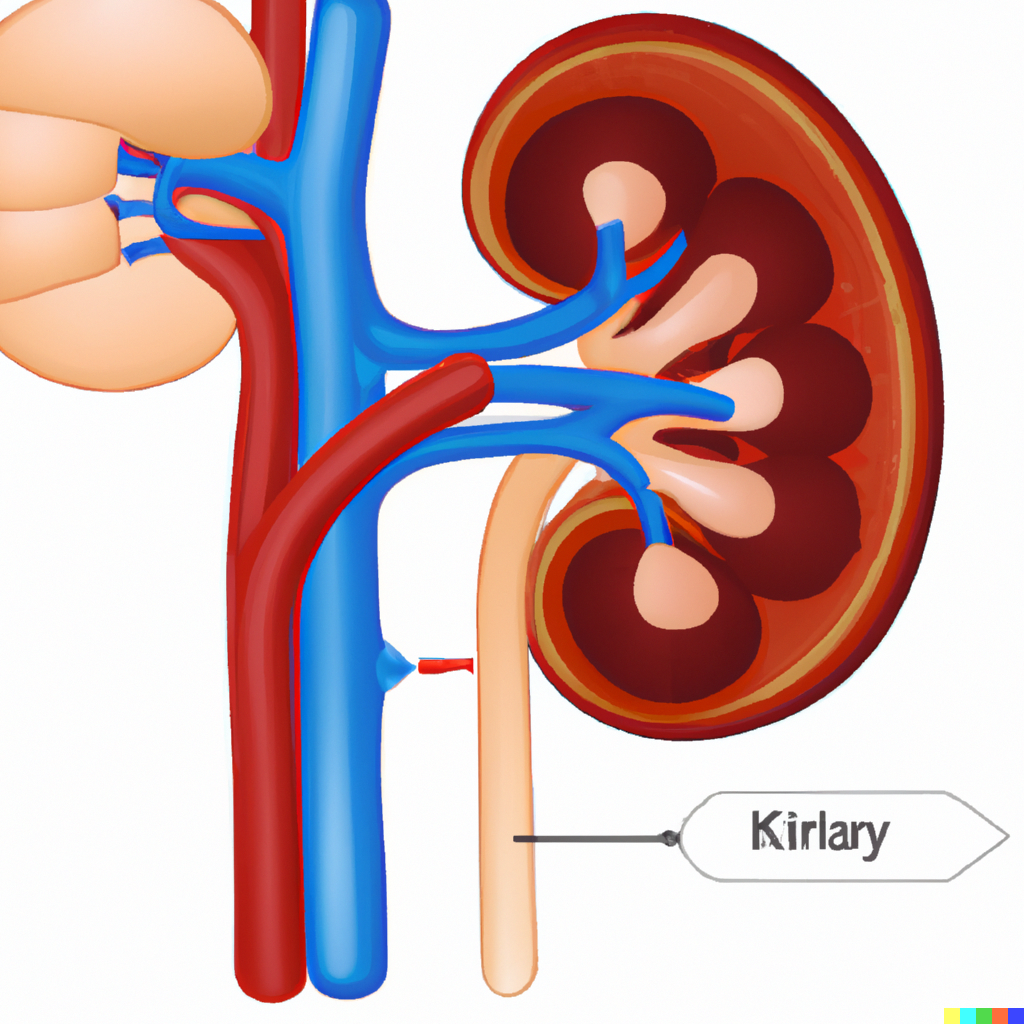
DECLARE-TIMI 58将17160名2型糖尿病患者、肌酐清除率>60毫升/分钟,以及动脉粥样硬化性心血管疾病(CVD;40.6%)或CVD风险因素(59.4%)随机分配到达格列净或安慰剂组。在基线、6个月、12个月和此后每年都对尿蛋白-肌酐比率(UACR)进行测试。UACR随时间的变化被作为连续和分类变量(≤15,>15至<30,≥30至≤300,以及>300 mg/g)按治疗组测量。综合心肾结果是估计肾小球滤过率(eGFR)持续下降≥40%至<60 mL/min/1.73 m2,终末期肾脏疾病,以及心血管或肾脏死亡;具体的肾脏结果包括除心血管死亡以外的所有结果。
结果共有16843名(98.15%)参与者纳入基线UACR:9067名(53.83%)≤15 mg/g,2,577名(15.30%)>15至<30 mg/g,4,030名(23.93%)30-300 mg/g,以及1,169名(6.94%)>300 mg/g。作为一个连续变量,与安慰剂相比,使用达格列净从基线到4.0年,所有UACR和eGFR类别都有所改善(所有P<0.0001)。
在基线UACR、6个月、1年、2年、3年和4年时,各治疗组的UACR变化情况
其中,达帕格列净与安慰剂相比,UACR持续确认≥1个类别的改善更为常见(OR=1.45[95% CI 1.35-1.56],P<0.0001)。在UACR≥30 mg/g的亚组中,使用达格列净可降低心肾结局(P<0.0125),所有UACR亚组的肾脏特异性结局均有所降低(P<0.05)。
在DECLARE-TIMI 58中,达格列净对各种基线UACR和肾脏特异性结果表现出有利的影响,包括蛋白排泄正常的患者。这些结果表明,SGLT2i在糖尿病肾脏疾病的初级预防中也有一定作用。
参考文献:
The Effect of Dapagliflozin on Albuminuria in DECLARE-TIMI 58. Diabetes Care 2021 Aug; 44(8): 1805-1815. https://doi.org/10.2337/dc21-0076
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















这个药不错
61
#Diabetes#
73
#糖尿病肾脏疾病#
89
#BET#
68
#DIA#
73
越来越多新药可以应用
90
谢谢MedSci提供最新的资讯
111
学习
116