Clin Cancer Res:新辅助免疫治疗可提高III-IVA期CSCC-HN患者的病理缓解率
2021-08-17 Nebula MedSci原创
新辅助免疫治疗可安全用于局部晚期、可切除的CSCC-HN患者,并能诱导较高的病理缓解率
局部进展、可切除的头颈部皮肤鳞状细胞癌(CSCC-HN)的标准疗法是手术后再予以放疗;但该疗法在美容和功能上可能是毁灭性的,而且许多患者会复发。
“Clin Cancer Res”杂志上近期发表的一项2期临床试验“Pilot Phase II Trial of Neoadjuvant Immunotherapy in Locoregionally Advanced, Resectable Cutaneous Squamous Cell Carcinoma of the Head and Neck”,评估了新辅助免疫疗法在这类患者中的疗效和安全性。
该试验招募了新确诊的或复发性III-IVA期 CSCC-HN患者,予以了两个疗程的新辅助PD-1抑制治疗。主要终点是根据RECIST 1.1的客观缓解率(ORR)。次要终点包括病理缓解率(病理完全缓解[pCR]和主要病理缓解[MPR])、安全性、DSS、DFS和OS。探索性终点包括缓解的免疫生物标志物。
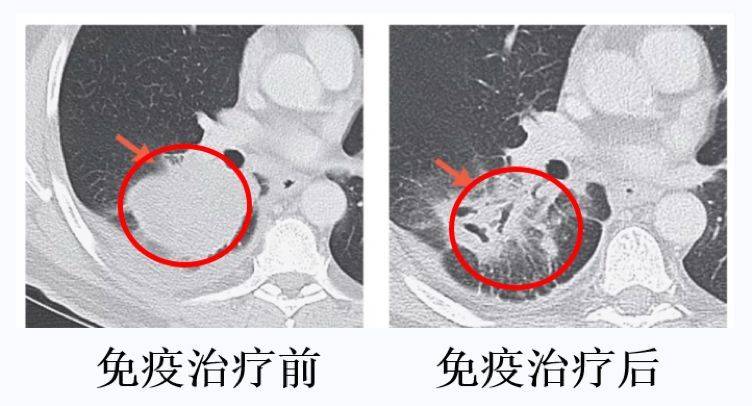
治疗后肿瘤体积的变化
共招募了20位患者,其中7位为复发性疾病。6位(30%)患者获得了部分缓解,14位(70%)获得了pCR(n=11)或MPR(n=3)。在新辅助治疗期间或治疗后未发生严重的不良事件(SAE)。
中位随访了22.6个月后,只有一位患者病情进展后死亡,一位患者非因病死亡,2位患者复发。12个月DSS、DFS和OS率分别是95%、89.5%和95%。
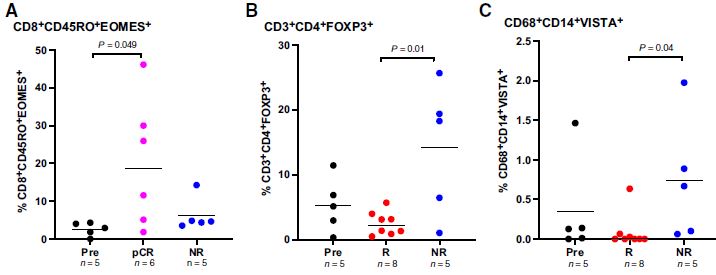
治疗前后有无缓解患者肿瘤微环境中的免疫细胞的数量
基因表达分析显示,获得pCR或MPR的患者存在炎性肿瘤微环境,而CyTOF分析显示,获得pCR的患者的记忆性CD8+T细胞显著富集。
综上,新辅助免疫治疗可安全用于局部晚期、可切除的CSCC-HN患者,并能诱导较高的病理缓解率。此外,病理缓解与炎性肿瘤微环境有关。
原始出处:
Renata Ferrarotto, et al. Pilot Phase II Trial of Neoadjuvant Immunotherapy in Locoregionally Advanced, Resectable Cutaneous Squamous Cell Carcinoma of the Head and Neck. Clin Cancer Res August 11 2021. DOI: 10.1158/1078-0432.CCR-21-0585

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#III#
71
#病理缓解率#
79
#新辅助#
90
#SCC#
69