胚胎不在意精子:阴道内精液注入不提升试管受精妊娠率!
2024-09-26 生殖医学论坛 生殖医学论坛 发表于上海
这项严谨且精心设计的研究表明,阴道内接触精浆并没有提高活产率。
In the simplest of terms, successful conception requires a healthy egg, sperm, and place for them to meet and grow. The past few decades have shown huge advancements in the success of in vitro fertilization (IVF); however, even under the best of circumstances, a quarter of seemingly healthy embryos do not implant, because of reasons that remain enigmatic. In an effort to chase these last remaining percentage points, every naturally occurring event in spontaneous conception is being analyzed to determine if they play an essential function in improved sustained implantation.
用最简单的话来说,成功受孕需要健康的卵子、精子和它们相遇和生长的场所。过去几十年,体外受精(IVF)的成功率取得了巨大的进步;然而,即使在最好的情况下,仍有四分之一看似健康的胚胎无法着床,其原因至今仍是个谜。为了争取这最后几个百分点,研究人员正在分析自然妊娠过程中的各个自然发生的事件,以确定它们是否在提高持续着床率方面发挥着至关重要的作用。
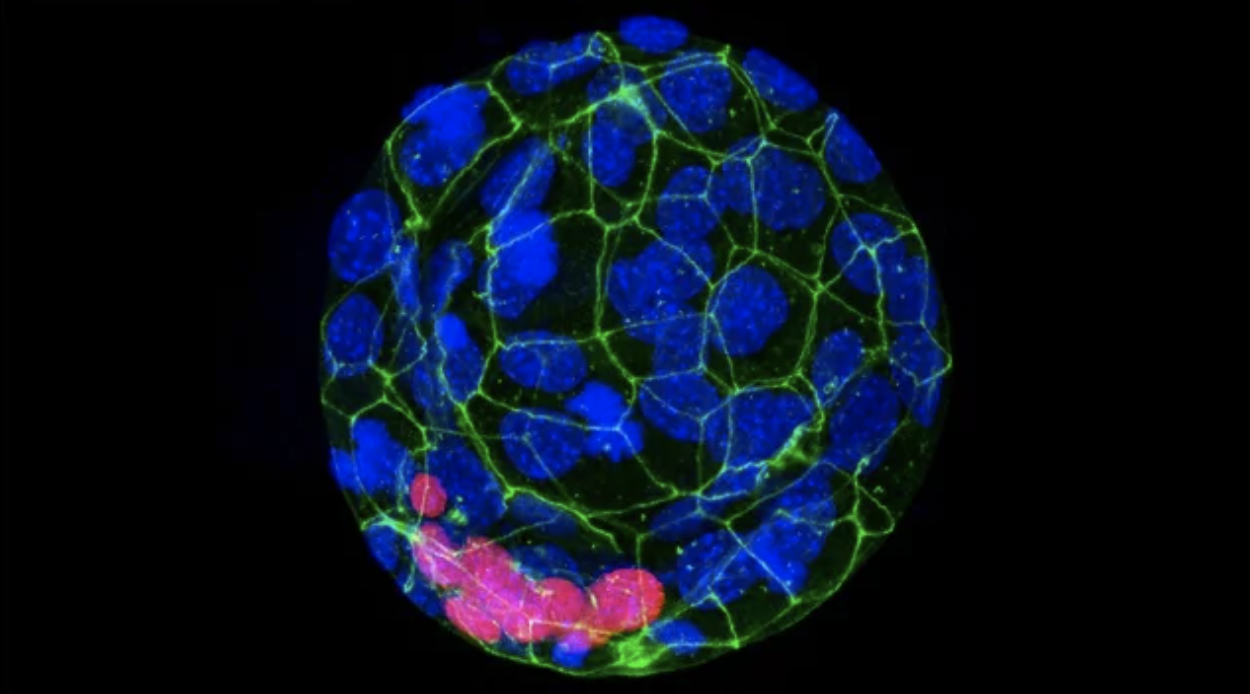
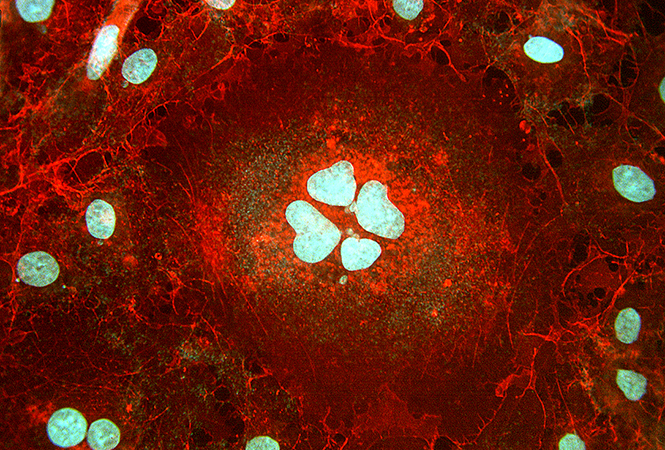
The optimal state of the endometrium for implantation is not understood perfectly. The role of semen exposure in embryo implantation has been investigated for many years, with the hypothesis that semen may cause physiologic changes in women that increase chances of successful pregnancy. There are thought to be hormonal, immunologic, and inflammatory influences. The role of immune system mediators, including histamine, prostaglandins, and macrophages, is a topic of current interest. It is believed that the implantation process modulates the body’s inflammatory response and that sperm can initiate this response (1). The mechanism is postulated to be through the release of prostaglandins that are found in the seminal fluid that commences a signaling cascade in a woman’s immune cells. The end result of this cascade is that the woman’s immune system becomes tolerant of the introduction of the embryo into the endometrium (2). These molecular level changes from semen that augment embryo implantation theoretically sparked the idea that IVF success could improve with introduction of semen to mimic the natural conception environment.
关于子宫内膜着床的最佳状态,我们还没有完全理解。多年来,人们一直在研究精液暴露对胚胎着床的作用,其中的假设是精液可能会引起女性身体的生理变化,增加成功怀孕的机会。这种变化被认为涉及激素、免疫和炎症因素。目前,免疫系统介质(包括组胺、前列腺素和巨噬细胞)的作用成为研究的热点。人们认为着床过程会调节身体的炎症反应,精子可以引发这种反应(1)。据推测,机制是通过精液中的前列腺素释放,这些前列腺素会启动女性免疫细胞中的信号级联。这个级联的最终结果是女性免疫系统对胚胎进入子宫内膜变得容忍(2)。精液在分子水平上的这些变化促进了胚胎着床,这从理论上激发了一种想法,即通过引入精液来模拟自然受孕环境,可能会提高体外受精的成功率。
Previously published data on the subject have been mixed. One 2017 meta-analysis that included 8 randomized control trials with over 2,100 patients demonstrated an increase in clinical pregnancy rate after embryo transfer with seminal plasma (relative risk [RR], 1.20; 95% confidence interval [CI, 1.04–1.39]), but found no significant difference in live birth rate (3). Similarly, another meta- analysis with 7 randomized controlled trials and 2,200 patients revealed a statistically significant improvement in clinical pregnancy rate (RR, 1.23; 95% CI, 1.06–1.42), but again no significant difference in live birth rate (4). Both commented on the lack of controlled methodology, variable quality of studies, and availability of data to determine clearly the impact on live birth rate. These prior studies highlight collectively the need for further investigation into the role of intravaginal seminal plasma in influencing live birth rates.
此前关于该主题发表的数据喜忧参半。2017年的一项荟萃分析纳入了8项随机对照试验,涉及2100多名患者,结果表明,使用精浆进行胚胎移植后,临床妊娠率有所提高(相对风险:1.20;95%置信区间:1.04–1.39),但还发现活产率并无显著差异(3)。同样,另一项包含7项随机对照试验和2200名患者的荟萃分析显示,临床妊娠率在统计学上有显著改善(相对风险:1.23;95%置信区间:1.06–1.42),但活产率仍然无显著差异(4)。这两项研究都指出了缺乏控制方法学、研究质量参差不齐以及数据可用性不足,从而无法明确确定对活产率的影响。这些先前的研究共同强调,有必要进一步调查阴道内精浆对活产率的影响。
The article entitled ‘‘Intravaginal exposure to seminal plasma after ovum pick up does not increase live birth rates after IVF or ICSI: a double-blind, placebo-controlled ran- domized trial,’’ published in the current issue of Fertility and Sterility, aims to rectify the ambiguity of the data regarding the influence of seminal plasma on live birth rates (5). This study was a double-blind, placebo-controlled, randomized controlled trial conducted at a single center in Sweden. The primary outcome of interest was live birth rate after fresh embryo transfer with intravaginal seminal plasma, powered to detect a 10% increase. To achieve this power, the study enrolled 393 couples in the seminal plasma group and 399 couples in the control group. Inclusion criteria were couples undergoing their first to third cycle of IVF with the broad diagnoses of female, male, combined, or unknown factor infertility. The stimulation protocols before transfer were either long agonist or antagonist (90.4%) with fresh day two (54.5%), three (15.2%), or five (31.3%) embryo transfers. For both groups, semen from male partners was collected on the day of oocyte retrieval after 2–3 days of abstinence. The semen was evaluated for total sperm count, sperm concentration, and sperm motility to ensure a healthy sample and then was processed to obtain seminal plasma. Directly after oocyte retrieval, both groups underwent deposition of fluid in the posterior fornix under ultrasound guidance, with the intervention group receiving at least 0.5 mL of semen supernatant and the control group receiving a saline solution.
本期《Fertility and Sterility》期刊刊登了一篇文章,题为 “卵子采集后阴道内接触精浆不会提高体外受精或细胞质内单精子注射(ICSI)后的活产率:一项双盲、安慰剂对照的随机对照试验”。该文章旨在纠正关于精浆对活产率影响的数据模糊不清的问题(5)。该研究是一项双盲、安慰剂对照的随机对照试验,在瑞典某中心进行。研究主要关注的结果是,使用阴道内精浆进行新鲜胚胎移植后的活产率,旨在检测活产率是否提高10%。为达到这一研究效力,研究纳入了393对夫妇进入精浆组,以及399对夫妇进入对照组。纳入标准为正在接受第一至第三个体外受精周期的夫妇,其广泛诊断为女性、男性、混合性或不明原因的不孕症。胚胎移植前的刺激方案为长效激动剂或拮抗剂(90.4%),其中新鲜胚胎移植时间为第2天(54.5%)、第3天(15.2%)或第5天(31.3%)。两组男性伴侣的精液均在禁欲2~3天后的取卵日收集。精液需进行总精子数、精子浓度和精子活力的评估,以确保样本健康,然后进行处理以获得精浆。在取卵后,两组均在超声引导下于阴道后穹窿处进行了液体沉积,其中干预组接受至少0.5毫升的精液上清液,而对照组接受生理盐水溶液。
Overall, the results were striking in that there was neither significant correlation between seminal plasma exposure and live birth rates nor any of the secondary outcomes including rates of positive pregnancy test, clinical pregnancy, miscarriage, and adverse events including infection. Regarding the primary outcome, live birth rate, the seminal and control groups had rates of 26.5% and 29.8% respectively, with a RR of 0.86 (CI, 0.70–1.07). Similarly, positive pregnancy test (RR, 0.93; 95% CI, 0.78–1.10) and clinical intrauterine pregnancy (RR, 1.00; 95% CI, 0.97–1.03) were not improved by intravaginal seminal plasma. This contrasts with the previously mentioned meta-analyses that had determined a benefit in clinical pregnancy rates.
总体而言,研究结果令人震惊,因为接触精浆与活产率之间并没有显著的相关性,与包括妊娠阳性率、临床妊娠率、流产率和包括感染在内的不良事件在内的所有次要结局之间也没有显著的相关性。关于主要结果活产率,精浆组和对照组的活产率分别为26.5%和29.8%,相对风险为0.86(置信区间:0.70-1.07)。同样,阴道内接触精浆并未提高妊娠试验阳性率(相对风险:0.93;95% 置信区间:0.78–1.10)和临床宫内妊娠率(相对风险:1.00;95%置信区间:0.97–1.03)。这与之前提到的确定有益于临床妊娠率的荟萃分析形成对比。
This rigorous, well-designed study demonstrated that there was no improvement in live birth rates with intravaginal seminal plasma exposure. The strengths of this study are that it is double-blind, with a placebo-controlled randomized design, large sample size, clearly delineated inclusion criteria, and control for confounding variables, and this study provides previously lacking robust data to support no significant improvement in live birth rates with seminal plasma. The broader impact of this study in the field of IVF is that it obviates the need for further investigation of intra- vaginal seminal exposure and can allow for future research to explore other mechanisms to influence endometrial receptivity to improve the rates of successful embryo transfer.
这项严谨且精心设计的研究表明,阴道内接触精浆并没有提高活产率。这项研究的优点在于它采用了双盲、安慰剂对照的随机设计,样本量大,纳入标准明确,并对混杂变量进行了控制。此外,该研究还提供了之前缺乏的可靠数据,以支持精浆对活产率没有显著提升的结论。这项研究在体外受精领域的更广泛影响是,它消除了对阴道内精液接触进行进一步调查的必要性,并允许未来的研究探索其他影响子宫内膜容受性的机制,以提高胚胎移植的成功率。
参考文献:
Embryos don’t care if the sperm is there—intravaginal semen deposition does not increase pregnancy rates in in vitro fertilization Pierpoint, Sara C. et al.Fertility and Sterility, Volume 122, Issue 1, 76 - 77
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#胚胎# #精子# #体外受精#
34