帕金森病(PD)是第二大最常见的神经退行性运动障碍。它的病理特征是黑质旁的多巴胺能神经元损失和含有α-突触蛋白聚集的细胞内包涵体。PD的临床谱系包括典型的运动症状和许多不太明显的非运动特征。
在中国,65岁以上人群的PD患病率为1.随着人口老龄化,预计到2030年中国将有约500万PD患者,占全球PD患者的一半,这将给社会和患者家庭带来沉重负担。
图1: 论文封面图
PD是一种具有异质性症状的进行性和复杂的神经系统疾病。PD的主要挑战是缺乏对疾病进展和异质性的了解,以及缺乏明确的疾病诊断、进展和预后的生物标志物。在全球范围内,过去10年已经开展了多项队列研究,进一步了解了该疾病的风险因素、病因、临床特征和自然史。
帕金森病最著名的研究队列是帕金森病进展标志物计划(PPMI),这是一项全面的观察性国际多中心研究,旨在确定帕金森病进展的临床、影像和生物标志物。然而,中国仍然缺乏大型多中心帕金森病队列研究,关于帕金森病自然史的数据有限。
为了解决这一问题并加强中国国内的合作,中南大学的湘雅医院的唐北沙等领衔建立了中国帕金森病及运动障碍多中心数据库和合作网络(PD-MDCNC),并启动了中国帕金森病注册中心(CPDR)。
这是一项大型的多中心、观察性、前瞻性队列研究,旨在探索中国帕金森病进展的临床和自然史特征、遗传结构、影像和生物标记。
CPDR在2018年1月至2020年12月期间,从中国的19个临床站点招募了PD患者。使用至少17个核心评估量表前瞻性地收集临床数据。通过每两年一次的面对面访谈对患者的临床结果进行随访。
他们在帕金森病和运动障碍多中心数据库和合作网络(PD-MDCNC)的基础上在中国启动了CPDR。
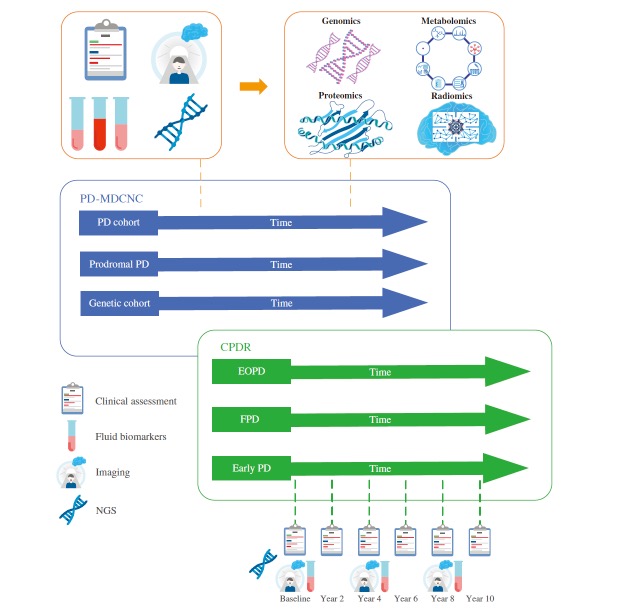
图2:论文结果图
共有3148名帕金森病患者入组,包括1623名男性(51.6%)和1525名女性(48.4%)。早发PD(EOPD,发病年龄≤50岁)和晚发PD(LOPD)的比例分别为897(28.5%)和2251(71.5%)。
按发病年龄分层显示,EOPD表现为较轻的运动和非运动表型,与运动障碍的概率增加有关。不同性别的比较表明,女性PD发病的平均年龄稍大,运动症状较轻,左旋多巴引起的运动障碍发生率较高。
CPDR是中国最大的多中心、观察性、纵向和自然历史的PD研究之一。它为扩大对PD进展的临床特征、遗传、影像和生物标志物的理解提供了机会。
原文出处:
Zhou X, Liu Z, Zhou X, et al. The Chinese Parkinson’s Disease Registry ( CPDR ): Study Design and Baseline Patient Characteristics. _Movement Disorders_. Published online May 3, 2022:mds.29037. doi:[10.1002/mds.29037](https://doi.org/10.1002/mds.29037)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#ERS#
105
#disorder#
77
#Disord#
72
#disorders#
77
#Dis#
63
加油!
59
#学习##梅斯医学科研互助群#
113
不错的文章
71
认真学习了
62
扩大对PD进展的临床特征、遗传、影像和生物标志物的理解提供了机会。
72