Eur Heart J:非阻塞性冠状动脉和阻塞性冠状动脉心肌梗死患者结局比较
2019-06-21 xing.T 网络
由此可见,这项研究证实了接受冠状动脉造影的老年MINOCA患者的预后不良,五分之一的MINOCA患者在12个月内出现了严重的不良事件。
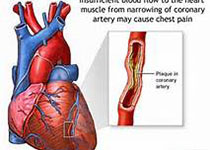
非阻塞性冠状动脉心肌梗死(MINOCA)患者的预后知之甚少。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员评估了MINOCA患者与冠状动脉疾病阻塞AMI患者(MICAD)的主要不良心脏事件(MACE),定义为全因死亡、急性心肌梗死(AMI)再次住院治疗、心力衰竭(HF)或AMI后12个月卒中。
研究人员对来自国家心血管数据登记处CathPCI登记中心(2009年7月至2013年12月)的AMI患者(≥65岁)进行了多中心、观察性队列研究,这些患者接受了冠状动脉血管造影,并与医疗保险和医疗补助中心(CMS)的数据进行联系。根据存在或不存在≥50%狭窄的心外膜血管将患者分类为MICAD或MINOCA。该研究的主要终点是12个月时的MACE,次要终点包括超过12个月时MACE组成疾病。
在286780名AMI入院者中,16849名患者(5.9%)为MINOCA。MINOCA患者12个月的MACE率(18.7% vs. 27.6%)、死亡率(12.3% vs. 16.7%)和AMI再住院率(1.3% vs. 6.1%)和HF(5.9% vs. 9.3%)与MICAD患者相比显著降低(P<0.001),但MINOCA和MICAD患者卒中再次住院治疗相似(1.6% vs. 1.4%,P=0.128)。在进行风险调整后,与MICAD患者相比,MINOCA患者在12个月内的MACE风险降低43%(风险比=0.57,95%置信区间为0.55-0.59)。对于调整后的MACE各种组成疾病的风险,这种模式类似。
由此可见,这项研究证实了接受冠状动脉造影的老年MINOCA患者的预后不良,五分之一的MINOCA患者在12个月内出现了严重的不良事件。
原始出处:
Rachel P Dreyer.et al.Myocardial infarction with non-obstructive coronary arteries as compared with myocardial infarction and obstructive coronary disease: outcomes in a Medicare population.JAHA.2019.https://doi.org/10.1093/eurheartj/ehz403
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阻塞#
123
#ART#
128
#患者结局#
105
#HEART#
110