脑出血是一种严重威胁人类健康的疾病,因其高发病率、高复发率和高致残率,给患者、家庭、社区乃至国家带来了沉重的负担。与西方国家相比,我国脑出血发病率更高。与缺血性卒中比较,脑出血急性期病死率更高,有效治疗手段更加有限。脑出血发病后仅不足20%的患者能够独立生活。目前,脑出血的病理生理机制尚不清楚,治疗方法有限。
随着MRI技术的不断发展,MRI检查逐渐被广泛应用于急性脑出血的临床诊断中,其具有明确定位、定性的优势。
脑内血肿的MRI信号一般演变规律:
一般可以把脑内血肿分为超急性期、急性期、亚急性早期、亚急性中期、亚急性晚期、慢性期。
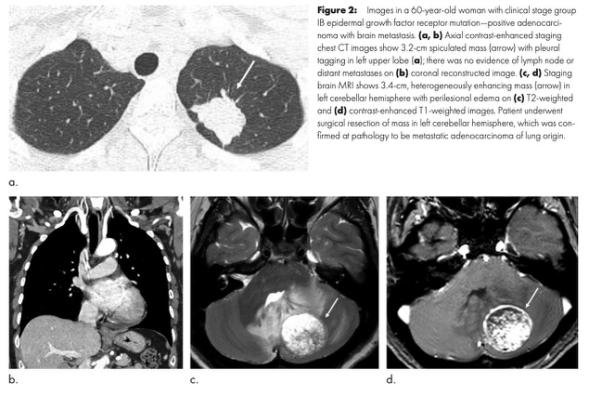
(一)超急性期是指出血的即刻,漏出的血液尚未凝固。实际上该期仅持续数分钟到数十分钟,临床上极少遇到。为含氧血红蛋白,对MR信号的影响轻微,超急性期尚未凝固的血液表现出血液的长T1长T2特性,因此在T1WI上表现为略低信号,在T2WI上呈现高信号,在FLAIR上也呈现高信号。

脑出血超急性期MRI表现
(二)急性期
一般为出血后2天内。在这一期红细胞的细胞膜保持完整,细胞内的氧合血红蛋白释放出氧变成脱氧血红蛋白。脱氧血红蛋白的顺磁性效应,造成局部磁场的不均匀,其外周环绕高信号水肿带。细胞内脱氧血红蛋白对T1值的影响较小,因此该期血肿在T1WI上信号变化不明显,常表现为略低信号或等信号,T2WI上表现为低信号,在FLAIR上也呈现低信号。血肿周围的水肿在MRI上表现为T1WI低信号,T2WI较高信号。
脑出血急性期MRI表现示意图与MRI影像
(三)亚急性早期
一般为出血后第3天到第7天。该期红细胞的细胞膜仍保持完整,细胞内开始出现正铁血红蛋白,因此该期也被称为正铁血红蛋白细胞内期,细胞内正铁血红蛋白的出现一般从血肿周边向中心逐渐发展。由于细胞内正铁血红蛋白具有较强的顺磁性,使血肿的T1值缩短,因此在T1WI上血肿从周边向中央逐渐出现高信号。该期血肿在T2WI上不表现为高信号,一般仍为低信号,在FLAIR上也呈现低信号。

脑出血亚急性早期MRI表现
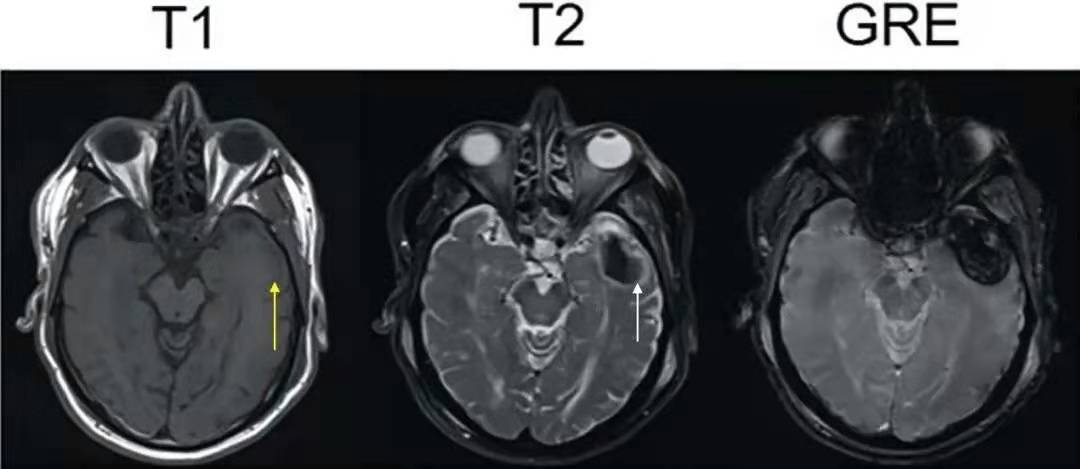
(四)亚急性晚期
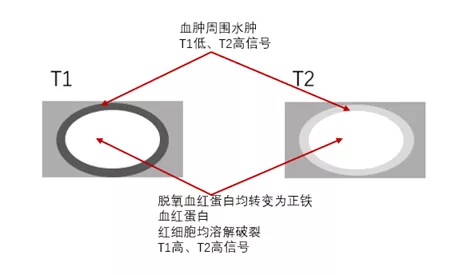
一般为出血后第7天到第14天。该期红细胞从血肿周边向中心逐渐开始溶解破裂,高铁血红蛋白分布于血肿液中。此时高铁血红蛋白仍然是那个和水亲密接触的顺磁性分子,没有一丝丝改变,所以对T1的影响不变,在T1像仍呈高信号。但是高铁血红蛋白从红细胞释放出来后,分布变得相对均匀,失去了磁场不均一性,因此局部磁敏感效应消失,T2缩短效应消失,在T2像呈现原本水肿液的信号,即高信号,在FLAIR上也呈现高信号。
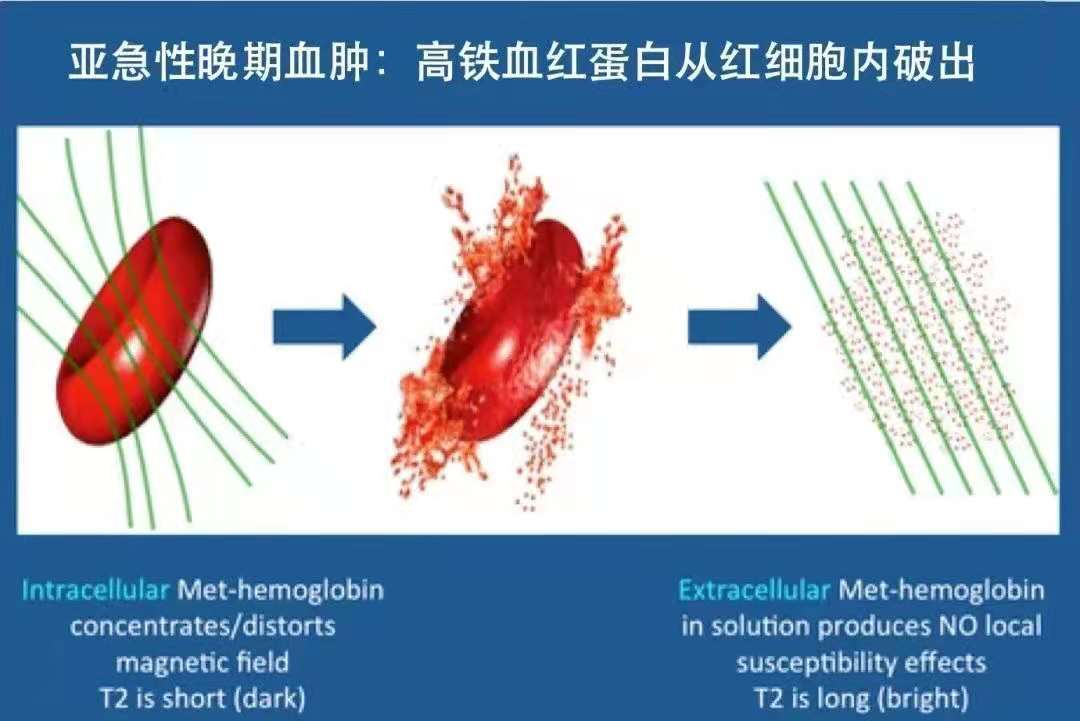
亚急性晚期血肿内局部磁敏感效应消失机制示意图
脑出血亚急性晚期MRI表现
(五)慢性期
一般为出血3周仍至数月以后。血肿逐渐吸收或液化,病灶周边的巨噬细 胞内有明显的含铁血黄素沉积。因此该期血肿逐渐演变为液化灶,在T1WI上为低信号,在T2WI上为高信号;周围的含铁血黄素在T2WI上表现为低信号环,在FLAIR上也呈现低信号。
脑出血的演变是一个复杂的过程,根据患者出血量的大小,患者的年龄,局部血液供应的好坏,脑出血吸收情况及分期时间并不相同,所以临床医生需要动态评估患者的疾病过程,对于磁共振表现给予合理的解读。
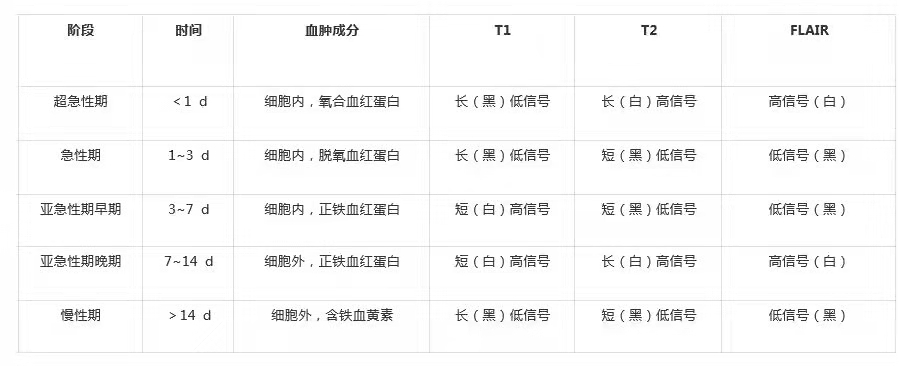
注:脑出血 MRI 信号变化各个分期并非有严格界限,是连续变化,此表格知识辅助学习,血液根据组织时间的演变,周围血管相通与否,都是不停演变的,需要灵活运用。
参考文献:
1、脑出血临床诊断思路和科研级专病病历建设,李琦,《中国医学前沿杂志(电子版)》
2、CT与 MRI检查在脑梗死并脑出血诊断中的价值研究,代媛代凤霞 李新胜,GuizhouMedicalJournal
3、脑出血各期 MRI特点及诊断,韩羽凤张子林 朱海波 ,长江大学学报
4、白人驹,张雪林. 医学影像诊断学.北京: 人民卫生出版社 (第3版).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















学习学习
109
学习了
89
#ICH#
165
#磁共振#
68
物理信号
107