Cardiovasc Diabetol:项目基线健康研究中糖尿病前期的多维表征
2022-08-22 从医路漫漫 MedSci原创
糖尿病前期包括血糖异常,包括空腹血糖受损、葡萄糖耐量受损和血红蛋白A1c (HbA1c)受损/升高
背景:糖尿病前期影响超过三分之一的美国人口,并与糖尿病和心血管疾病(CVD)的风险增加以及更高的医疗保健利用率和成本相关。然而,糖尿病前期包括血糖异常,包括空腹血糖受损、葡萄糖耐量受损和血红蛋白A1c (HbA1c)受损/升高,以及广泛的临床、化学、分子和病理生理异常,这些异常与进展为更严重和临床可识别的糖尿病和CVD的各种风险相关。识别美国普通人群中与不同血糖状态(正常血糖控制、糖尿病前期和糖尿病)相关的异常可能有助于识别发展和进展为更严重疾病状态的因果途径。此外,根据临床、化学、分子和病理生理学数据,识别与“高危”糖尿病前期相关的异常,或与进展为糖尿病/CVD和并发症的更高风险相关的特征,将允许更有针对性和更有效的预防干预。
项目基线健康研究(ClinicalTrials.gov NCT 03154346)(PBHS)是一项独特的、多中心、前瞻性队列研究,利用先进的技术和数字能力进行招募和数据收集。PBHS研究在亲自研究访问中进行了深度表型分析,包括病史、身体功能测量、成像和生物样本收集,以及纵向数字健康数据、调查数据和年度随访。
目的:虽然糖尿病前期已经通过传统的队列研究进行了描述,但在本研究中,我们使用PBHS研究中收集的各种新方法,将糖尿病前期参与者与血糖控制正常或患有糖尿病的参与者进行了比较。此外,我们确定了与糖尿病前期进展为糖尿病以及糖尿病前期逆转为正常血糖控制相关的生物标志物。
方法:项目基线健康研究(PBHS)是一项对2502名成年人进行的多地点前瞻性队列研究,通过影像学、实验室检查、临床评估、病史、个人设备和调查进行深入的临床表型分析。参与者在每次访视时根据血糖、HbA1c、药物和自我报告按糖尿病状态(糖尿病[DM]、糖尿病前期[preDM]或无糖尿病[noDM])进行分类。执行主成分分析(PCA)以创建使用线性模型跨组进行横断面比较的因素。使用逻辑回归来确定与从preDM进展到DM以及从preDM逆转到noDM相关的因素。
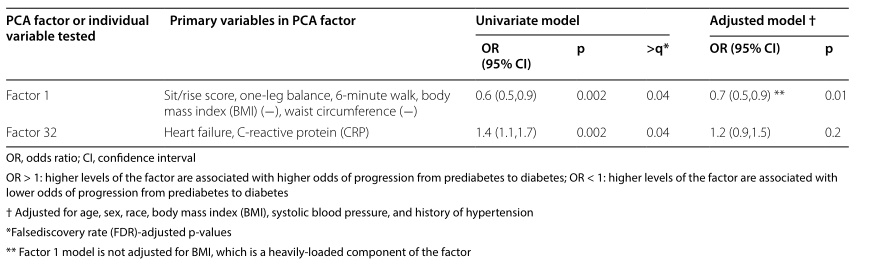
结果:在登记时,1605名参与者患有noDM544人患有preDM352人患有糖尿病。经过4年的随访,52名preDM患者发展为DM,153名患者恢复为noDM。主成分分析确定了33个因素组成的临床变量集群;这些与八个被先验地确定为感兴趣的个体变量一起被测试。在多重比较的错误发现率调整后,noDM与preDM和DM之间的六个PCA因子和六个先验变量显著不同(q < 0.05)。其中,两个因素(一个包括葡萄糖测量,一个包括人体测量和身体功能)显示了各组之间的单调/分级关系,三个先验变量也是如此:ASCVD风险、冠状动脉钙和甘油三酯(所有q < 10-21)。四个因素在preDM和noDM之间有显著差异,但在DM和preDM之间一致或相似:红细胞指数(q = 8 × 10-10)、肺功能(q = 2 × 10-6)、慢性疾病风险(q = 7 × 10-4)和心脏功能(q = 0.001),以及舒张功能(q = 1 × 10-10)、睡眠效率(q = 9 × 10-6)和睡眠时间(q = 6 × 10-5)的先验变量。两个因素与糖尿病前期进展为糖尿病相关:人体测量和身体功能(OR [95% CI]: 0.6 [0.5,0.9],q = 0.04),心力衰竭和c-反应蛋白(OR [95% CI]: 1.4 [1.1,1.7],q = 0.02)。人体测量和身体功能因素也与从糖尿病前期到noDM的逆转相关:(OR [95% CI]: 1.9 [1.4,2.7],q = 0.02)以及白细胞指数因素(OR [95% CI]: 0.6 [0.4,0.8),q = 0.02),以及先验变量ASCVD风险评分(OR [95% CI]:as CVD评分每增加0.1,q = 0.02为0.7 [0.6,0.9])和甘油三酯(OR[95% CI]:每增加25 mg/dl,q = 0.05为0.9 [0.8,1.0])。
表1项目基线健康研究(PBHS)队列的基线特征
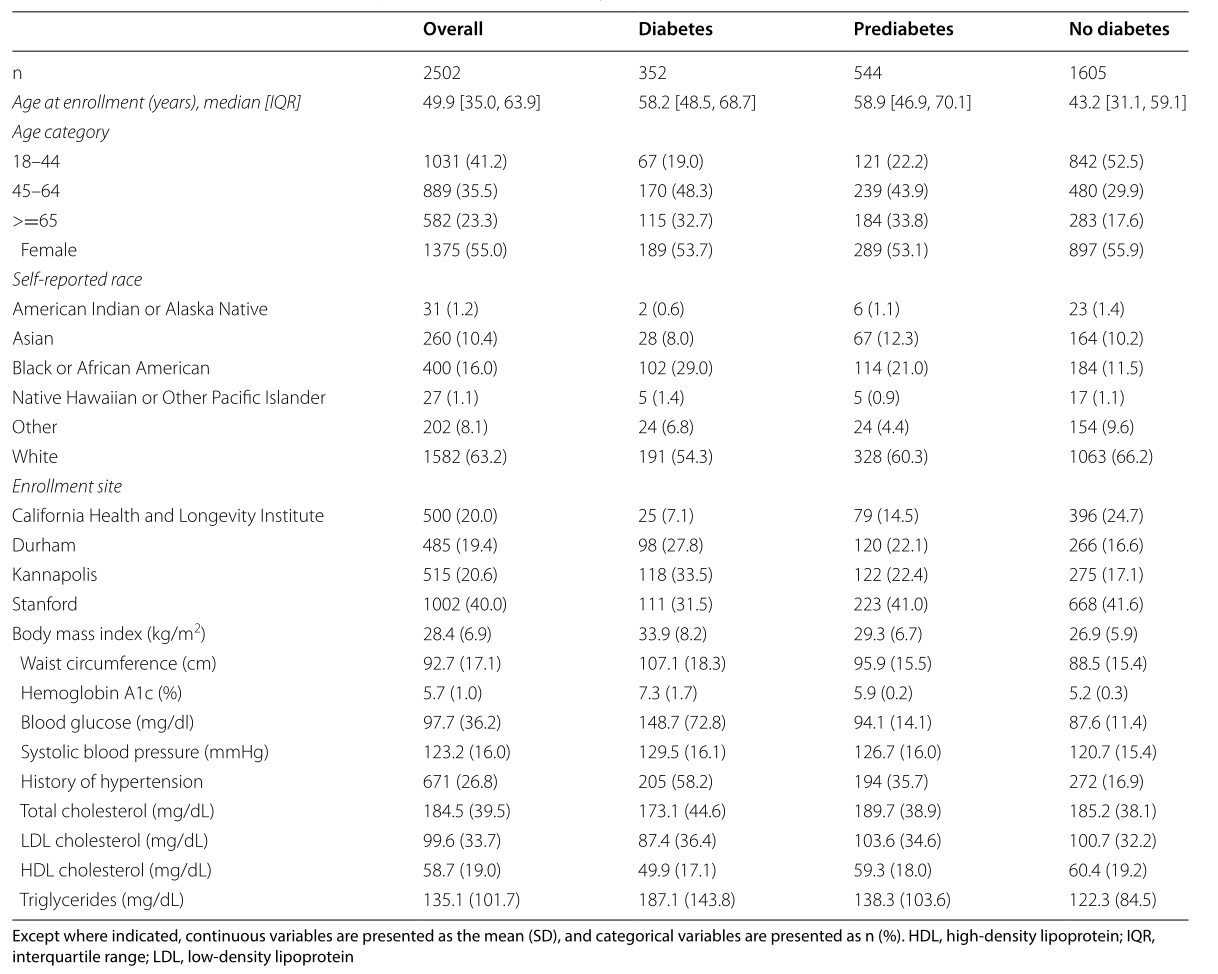
表2主成分分析因子的构成
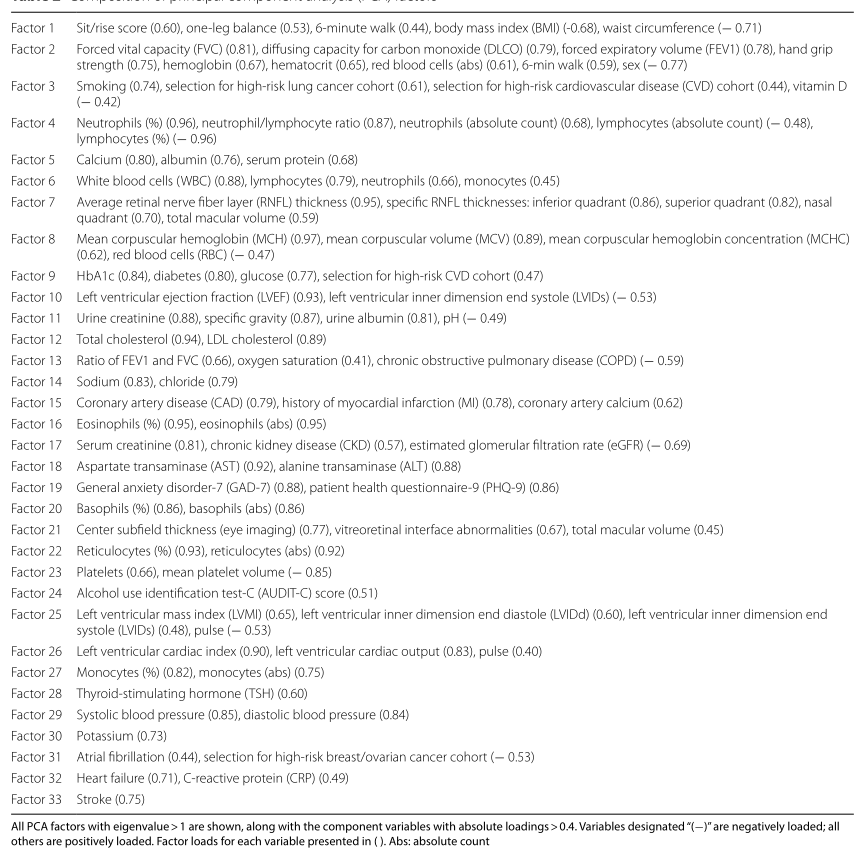
表3与糖尿病组显著相关的PCA因子,按总体显著性排序
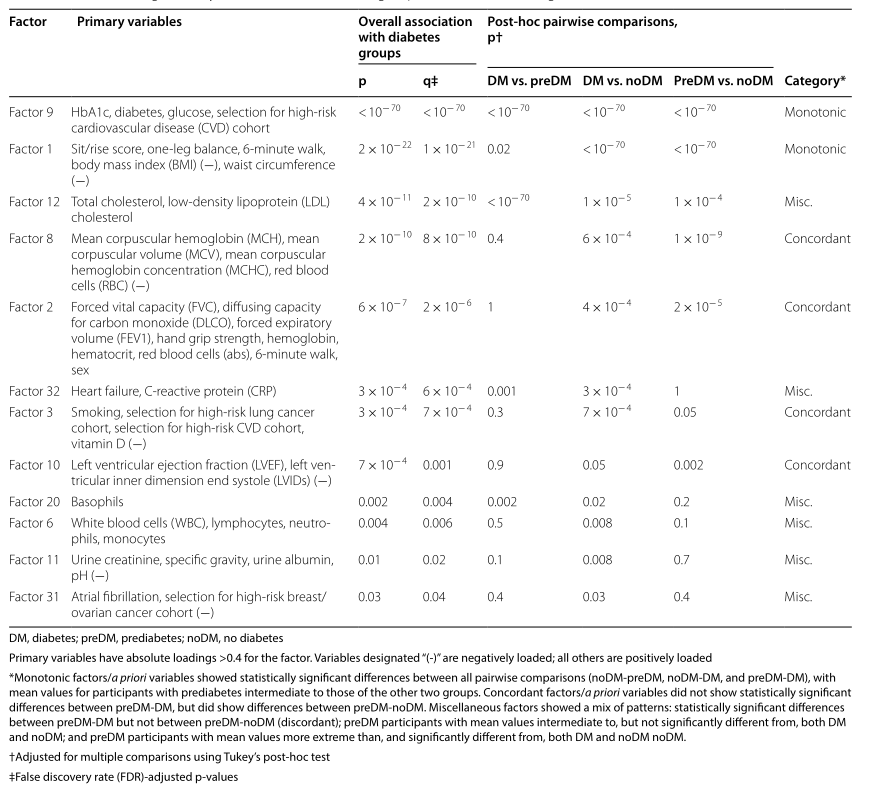
表4先验定义的与糖尿病组相关的个体变量,按总体显著性排序
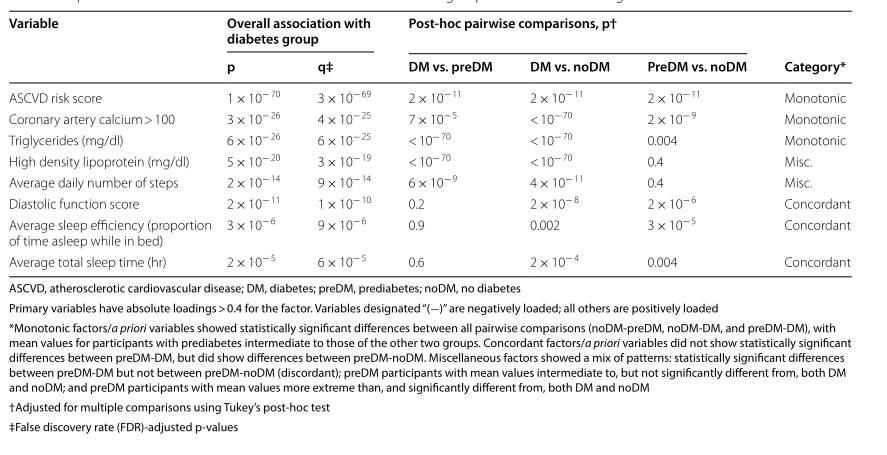
表5与糖尿病前期进展为糖尿病相关的因素和个体先验变量
结论:患有preDM的PBHS参与者在DM前表现出心脏、肺和血液学指标的病理生理学变化以及身体功能和睡眠指标的下降;一些变化预示着进展为糖尿病的风险增加。测量人体指标和身体功能的因素是与进展为糖尿病和逆转为非糖尿病性糖尿病相关的最重要因素。未来的研究可能会确定这些变化是否阐明了进展为糖尿病和相关并发症的途径,以及它们是否可用于识别进展为糖尿病的高风险个体,以进行有针对性的预防干预。
原文出处:Chatterjee R, Kwee LC, Pagidipati N, et al.Multi-dimensional characterization of prediabetes in the Project Baseline Health Study.Cardiovasc Diabetol 2022 Jul 18;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BET#
63
#DIA#
51
#ASC#
47
#健康研究#
72