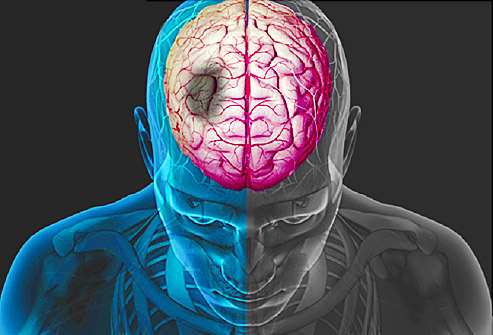
Sci Rep:心率变异性的复杂性可预测急性缺血性卒中患者卒中演变
2015-12-04 MedSci译 MedSci原创
早期评估心率变异性的复杂性可以作为入住ICU的non-AF 缺血性卒中患者卒中演变的预测因素。
国立台湾大学医院卒中中心和神经内科Sung-Chun Tang研究发现心率变异性的复杂性可以预测急性缺血性卒中患者卒中演变。研究结果2015年12月1日在Scientific Report在线发表。
背景: 大约三分之一的急性卒中患者可能经历卒中演变,通常会导致更差的结果。最近研究表明MSE(multiscale entropy ,多尺度熵),一种HRV(heart rate variability,心率变异性)分析的非线性方法是non-AF(non-atrial fibrillation,非心房颤动)卒中患者预后的一个早期预测因素
目的: 研究旨在进一步调查MSE是否可以作为SIE(进展性卒中)的预测方法。
方法: SIE被定义为入院3天内NIH健康卒中量表评分≥2分。在患者入院后的第一个24小时内连续测量 1小时心电图信号,使用MSE分析HRV。HRV复杂性指数定义为MSE曲线下面积。
结果:研究共纳入90例入住ICU的non-AF缺血性卒中患者。19例(21.1%)患者符合SIE标准。与没有演变为SIE的患者相比,演变为SIE的患者HRV复杂性指数数值显著降低(21.3±8.5 vs 26.5±7.7,P=0.012)。调整临床变量后,复杂性指数数值更高的患者演变为SIE的可能性显著减少(OR 0.897,95%CI 0.818-0.983,P=0.020)。
结论:早期评估心率变异性的复杂性可以作为入住ICU的non-AF 缺血性卒中患者卒中演变的预测因素。
原始出处
Chih-Hao
Chen, Pei-Wen Huang, Sung-Chun Tang, et all. Complexity of Heart Rate
Variability Can Predict Stroke-In-Evolution in Acute Ischemic Stroke Patients. Scientific
Report. Published online 01 December 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#缺血性卒#
0
#演变#
102
#缺血性#
71
#缺血性卒中患者#
96
好文章,值得收藏
157
好文章,值得收藏
148
#卒中患者#
54
#变异#
55
#心率变异性#
114
#复杂性#
69