Neurology:追踪3年,脑卒中后1年期脑白质高信号体积与同时期认知评分密切相关!
2022-03-05 Naomi MedSci原创
脑卒中发生后,波动的脑白质高信号(WMH)显示,1年中而非基线,WMH量与同时期的认知评分密切相关。 纵向协变卒中后认知和日常活动独立性的下降是痴呆诊断的核心,与WMH量的增加有关。
脑小血管疾病(cerebral small vessel disease,SVD)在卒中患者中很常见,是卒中和血管性痴呆的常见原因。脑小血管疾病的一个关键特征——脑白质高信号(white matter hyperintensity,WMH),已被证明在脑卒中、认知功能受损、老年社区居民的神经或认知症状的调查、平均年龄63岁的健康成年人增加或减少。目前尚不清楚 SVD 病变发生的时间与卒中、痴呆的临床发展有何关系。
诊断痴呆症,需要同时满足认知能力和日常生活能力下降。卒中后通常根据改良 Rankin 量表(mRS)测量的卒中后残疾程度来定义功能状态,即完成日常生活活动的独立程度。“轻度神经认知障碍”与“重度神经认知障碍”的区别在于依赖性增加。 这在卒中后尤为重要,因为在轻度卒中3年后,mRS 恶化和认知障碍都很常见且相互关联。然而,尚不清楚 SVD 进展是否会影响这些障碍的相互作用。
在横断面研究中,卒中出现时白质高信号 (WMH) 恶化与当前或长期评估的认知恶化有关。然而,尚不清楚WMH的纵向变化是否预测卒中后认知或功能减退。评估 WMH 进展和卒中后认知下降的小型MRI 研究未发现纵向关联,但随访样本量可能不足,样本范围n从30到94不等。此外,最近研究表明,WMH可长期减少或增加,尽管对于原因尚知之甚少,但纵向研究并未考虑 WMH 的波动。尽管许多研究评估了卒中后 WMH 和 mRS 的基线变化,但尚不知道有任何研究评估了卒中后 WMH 进展和 mRS 变化,或WMH 进展或严重程度是否在特定时间点是否影响 mRS和卒中后认知能力的变化,尽管相关研究正进一步探究中。
当前的深入分析建立在Mild Stroke Study-2——关于卒中后1年和3年预后的研究,其中包括认知预测因子和认知-mRS 关系,但没有评估包含认知、mRS 和 WMH 的3个要素的纵向变化。近日,有研究人员旨在确定 WMH 与认知、mRS 的关联是否在卒中后的不同时间点发生变化; 关联是否因个体内部轨迹而异;纵向 WMH 体积变化是否与认知变化、mRS 作为共同主要、共同变化的终点相关;以及是否有任何关联更强烈地推动认知或 mRS 的变化。
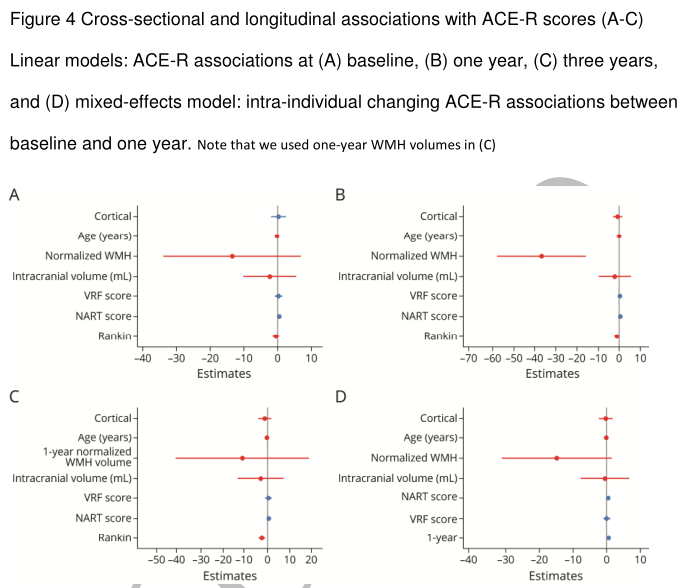
在轻微缺血性卒中发生后3个月内招募了患者,定义为 NIHSS 评分 <8,并且预计不会导致改良的 Rankin 评 (mRS)>2。 参与者在1年内反复接受MRI,并在1年和3年内反复进行认知和 mRS 评估。运行了纵向混合效应模型来评估 Addenbrooke 的认知考试修订版 (ACE-R) 和修改后的 Rankin 的变化分数(mRS)。对于mRS,评估了纵向 WMH 体积(立方根;颅内体积百分比 [ICV]),调整了年龄、NIHSS、ACE-R、卒中亚型和评估时间。 对于 ACE-R,还针对 ICV 进行了调整,mRS、病前智商和血管危险因素。然后,使用多变量模型来联合评估不断变化的认知/mRS,并使用所有可用数据针对预后变量进行调整。
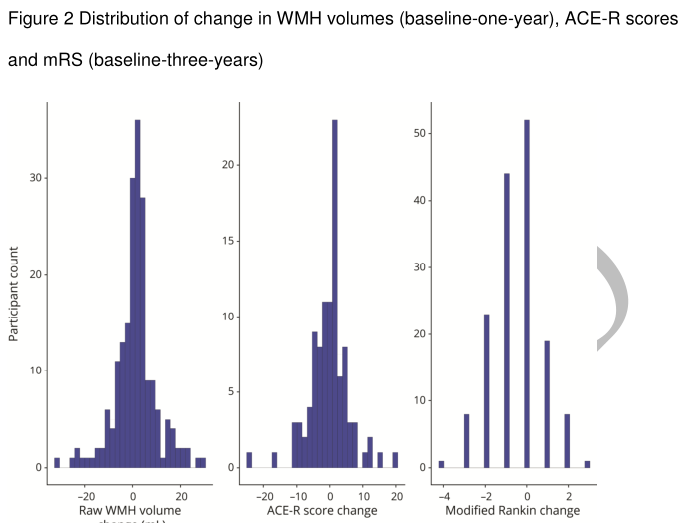
- 共招募了 264 名患者;平均年龄为 66.9(标准差 11.8);41.7% 是女性;中位 mRS 1 (IQR 1-2)。
- 卒中1年后,相比较于亚急性 WMH 体积和 ACE-R (β=0.105, 95%CI -0.265 to 0.054, p=0.195),标准化 WMH 体积与1年 ACE-R 的相关性更强(β= -0.259,95% 置信区间 [CI] 每 1 点 ACE-R 降低 WMH -0.407 至 -0.111,p=0.001 )。
- 3年期 mRS 与3年期 ACE-R 相关(β=-0.272,95%CI -0.429 至 -0.115, p=0.001)。
- 基线1年中联合评估ACE-R/mRS 的综合变化与 WMH 体积波动相关的(F=9.3,p=0.03)。
卒中发生后,波动的 WMH 显示,一年中而非基线,WMH体积与同时期的认知评分密切相关。 纵向协变卒中后认知和独立性的下降是痴呆诊断的核心,与WMH量的增加有关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#卒中后#
99
#高信号#
95
#Neurol#
81
#白质#
71
dd
97
#白质高信号#
83
#脑白质高信号#
86