ST-T改变、T波倒置就是心肌缺血冠心病吗?
2020-05-13 网络 网络
临床上遇到心电图T波倒置、ST-T改变,第一印象就是心肌缺血,那么这种心肌缺血表现的心电图就一定是冠心病吗?
临床上遇到心电图T波倒置、ST-T改变,第一印象就是心肌缺血,那么这种心肌缺血表现的心电图就一定是冠心病吗?
其实不然,心尖肥厚型心肌病就是心肌缺血表现的非冠心病疾病之一。
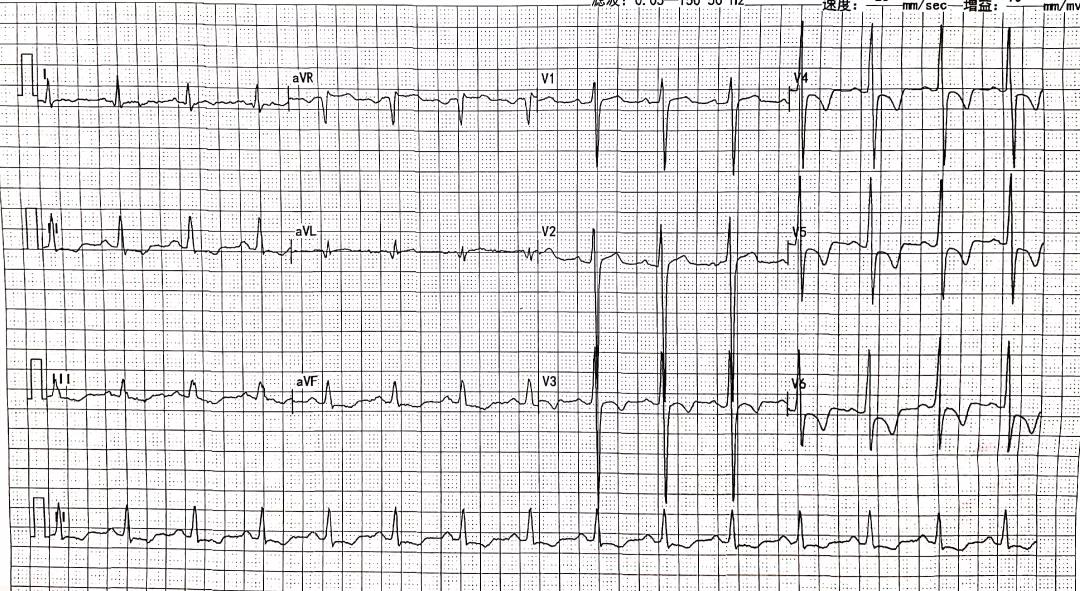
看到这个心电图你会想到什么呢?
心尖肥厚型心肌病(ApHCM)是原发性肥厚型心肌病中的特殊类型,主要局限于左心室乳头肌水平以下的心尖部肥厚。
ApHCM首先由日本学者Yamaguchi等于1976年报告;占肥厚型心肌病的25%左右、发病年龄30~50岁居多、男性多于女性。
ApHCM与经典的肥厚型心肌病不同,常不伴有左心室流出道动力性梗阻和压力阶差。肥厚的心肌主要位于前侧壁心尖处,而室间隔基底部多无肥厚。
1
临 床 表 现
症状:多数患者无症状或轻微症状。部分患者可有胸痛、心悸、呼吸困难、晕厥。心律失常可导致晕厥发生。由于舒张功能下降,心室充盈压升高,左房增大,晚期可导致舒张性心衰,出现呼吸困难、活动耐力下降及肺水肿。
体征:由于心尖肥厚型心肌病一般不伴有左心室流出道狭窄和压力阶差,对血流动力学影响下, 故无明显体征改变。
2
辅 助 检 查
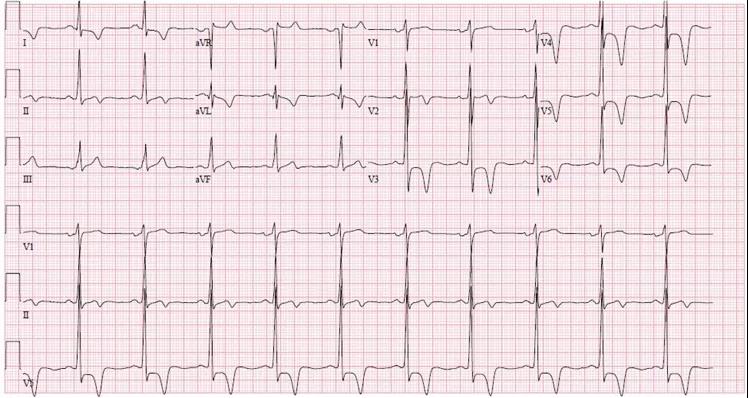
1. 心电图
对称性巨大倒置T波是AHCM的特征性心电图表现,主要出现在中胸及左侧胸前导联,最深可达4mV以上,典型时TV4>TV5>TV6,左心前导联QRS波高电压(Rv5>26 mm或Sv1+Rv5>35 mm),呈Rv4≥Rv5>Rv3的规律变化。
运动时,巨大倒置T波可出现变浅或变为直立等“伪正常” 改变,同时可伴有ST段水平型或下斜型下移0.05~0.40 mV。
ST段下移与T波倒置的导联可以不一致,但ST段下移程度与T波倒置深度呈正相关;
可有不同程度的胸前导联ST段压低,V2~V5最常见;
部分患者有QTc延长;
一般无异常Q波出现。
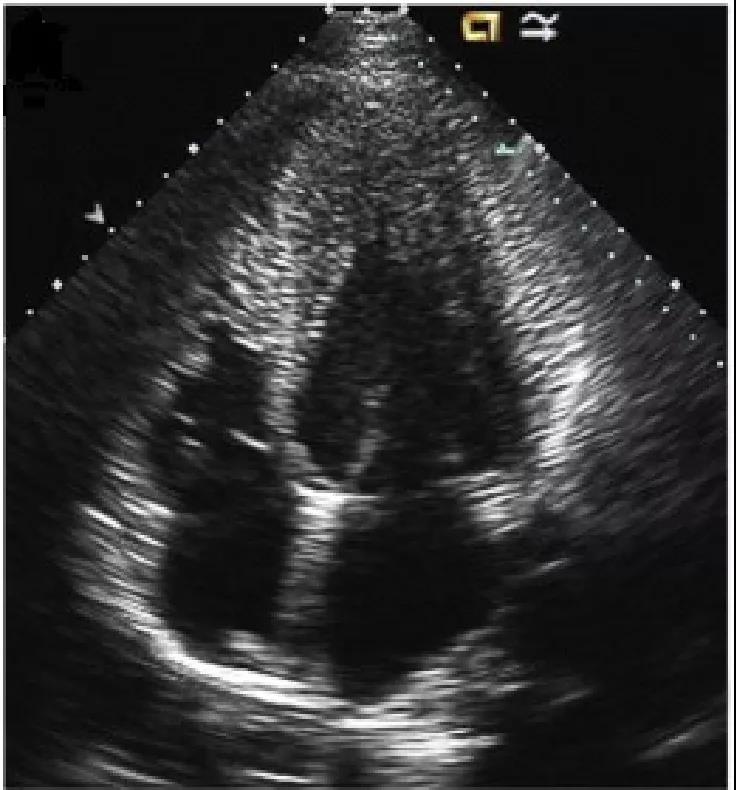
2. 超声心动图:
可检出心肌肥厚的部位及程度,通常肥厚≥15 mm。
3. 左室造影:
对心尖肥厚型心肌病患者行右前斜30°左心室造影可见舒张期左心室呈特征性“黑桃样”形改变,心尖部心肌明显肥厚;
收缩期可见心尖腔部位完全闭塞。

似扑克牌“黑桃”形改变,尖部向右下
4. MRI:
表现心尖部位的心肌肥厚,舒张期末见心尖部黑桃样改变,收缩期末见心尖腔完全消失。
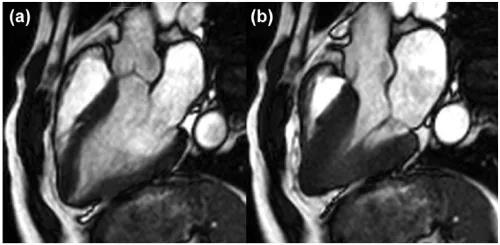
左(a)舒张期;右(b)收缩期
5. 动态心电图
所有HCM患者应接受24-48小时的动态心电图监测,以评估室性心律失常和SCD风险;
确定心律失常是否是心悸或晕厥的原因;
Holter监测记录到非持续性室速意味着SCD的风险增加。
3
诊 断
多发生在中青年患者,男性多于女性,可出现胸痛、活动耐量下降、头晕、心悸等症状;
心电图心前导联见巨大倒置T波和QRS波高电压;
影像学检查见舒张期左心室呈特征性“黑桃样“,收缩期显著的心尖腔消失;
无左心室流出道梗阻的血液动力学改变;
无高血压、冠心病或其他类型心肌病证据者即可确诊为心尖肥厚型心肌病。
4
主要的鉴别诊断
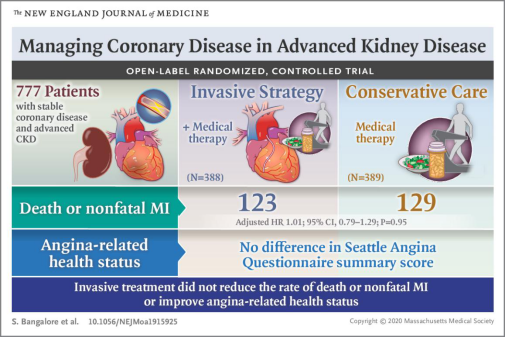
1. 冠心病
常有高脂血症、糖尿病、高血压等危险因素,有典型心绞痛的表现,心电图有ST- T 动态改变,一般无无R波增高/左室高电压,主要通过冠脉CTA或造影鉴别,心尖肥厚型心肌病冠脉CTA或造影无异常。
2.高血压性心脏病
长期高血压可导致左室肥厚,但左室壁肥厚很少超过15mm,且心肌肥厚通常呈对称性 。心电图可存在左室肥厚伴劳损。常伴有其他靶器官损害的证据,如慢性肾脏、眼底改变等。
3.运动员心脏
规律强化体能训练可致左室室壁轻度增厚,心超常示左心室腔内径增大、室壁轻度均匀增厚,通常13-15 mm,通常不合并左房增大、严重的左室舒张功能异常和收缩速度降低。家族史、心电图和左室腔大小可有助于鉴别。
以上为主要鉴别,其他如限制性心肌病、淀粉样变等疾病也会表现为心肌肥厚。
5
治 疗
β受体阻滞剂:可减少心肌耗氧量、改善舒张功能,缓解心绞痛等症状;
钙离子拮抗剂:多选用维拉帕米,对于无法耐受β受体阻滞剂或有禁忌症者,建议使用维拉帕米以缓解症状;
合并房颤者:均建议口服抗凝药;
对于SCD风险高者,置入ICD预防猝死;
嘱咐患者注意休息,适当运动(慢跑游泳等有氧运动)避免剧烈运动;
长期随访,半年到一年心内科检查,调整用药剂量、检查心超等,观察用药后能否延缓或抑制心室进一步肥厚;
6
经验及总结
心尖肥厚型心肌病心电图有ST-T变化,易被误诊为冠心病;
心尖肥厚性心肌病的ST-T改变不是缺血导致的,主要是由于心室的除极过程发生改变所致的复极异常,且多数不会有明显的动态变化;
超声心动图是确诊本病的有效易行的手段;
如果临床见到类似心电图,而患者无典型的心绞痛,心肌损伤标志物正常,发作时及缓解后的心电图无明显的变化,则首先考虑有无 ApHCM的可能。
本病有遗传倾向,需要观察家族成员是否有类似疾病。
专家简介

陈瑞珍 教授
陈瑞珍,医学博士,博士生导师。复旦大学附属中山医院心内科教授、上海市心血管病研究所中心实验室副主任。教育部新世纪优秀人才计划入选者,上海市优秀学术带头人。
主要从事内科心血管疾病的临床与基础研究,尤其是对心肌炎、心肌病、心力衰竭、高血压等有长期深入的研究。主持国家自然科学基金课题6项、作为负责人或主要PI承担国家及省部级科研课题20余项。在Circulation、Circulation Research、Europe Heart Failure、J Viol、IJC等杂志发表SCI收录论著70余篇。曾获国家科技进步二等奖、省部级科技进步奖十余项。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#T波倒置#
64
学习了
134
repost
152
zxd
132
点赞👍
146
嗯
148
#ST-T改变#
61
学习了
91
好
70